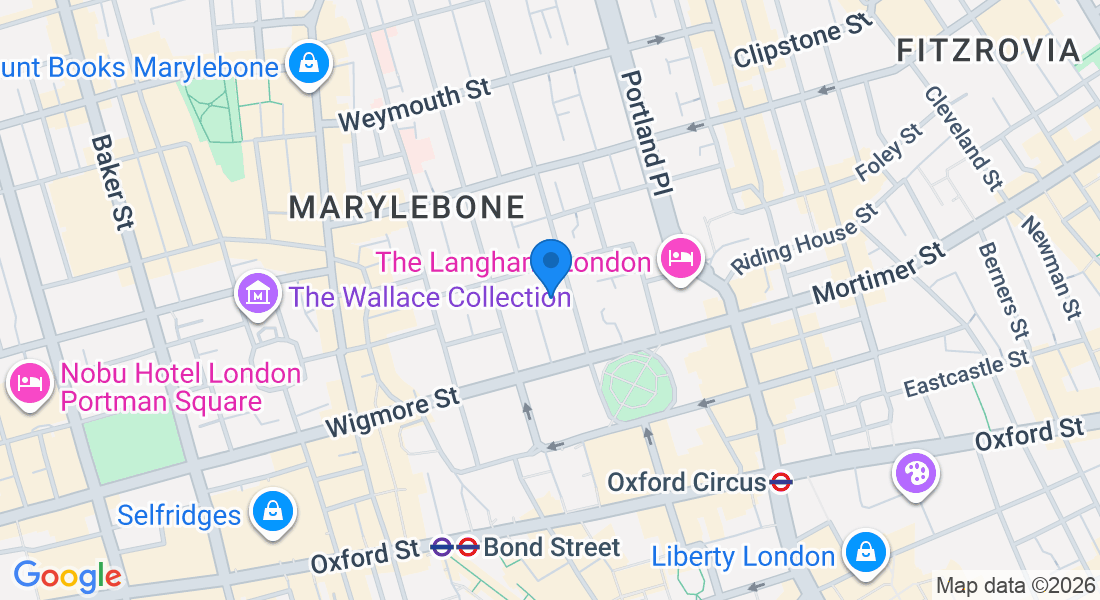
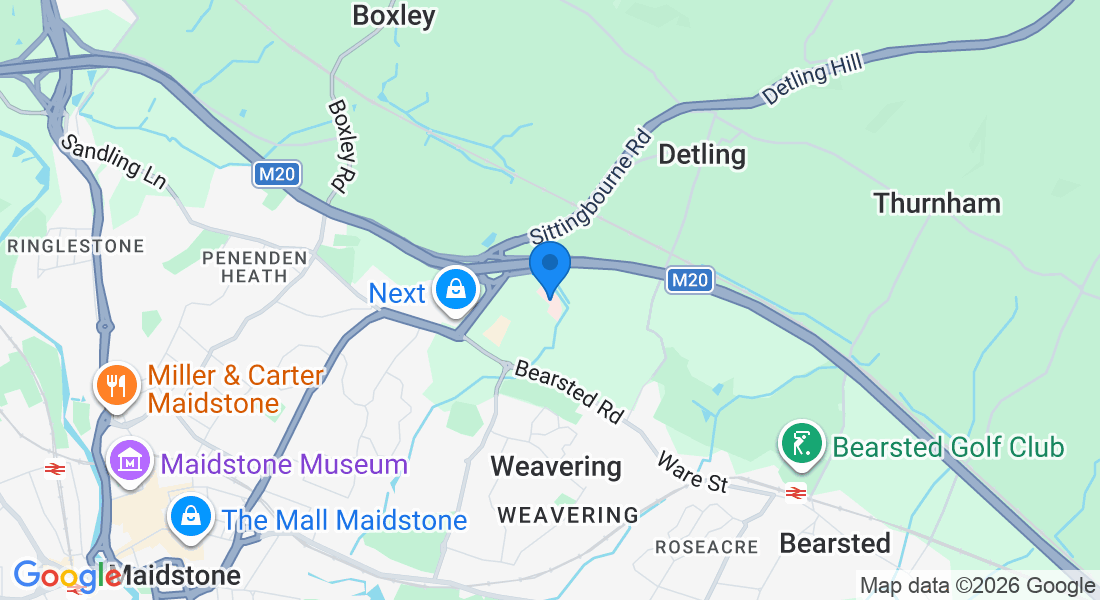
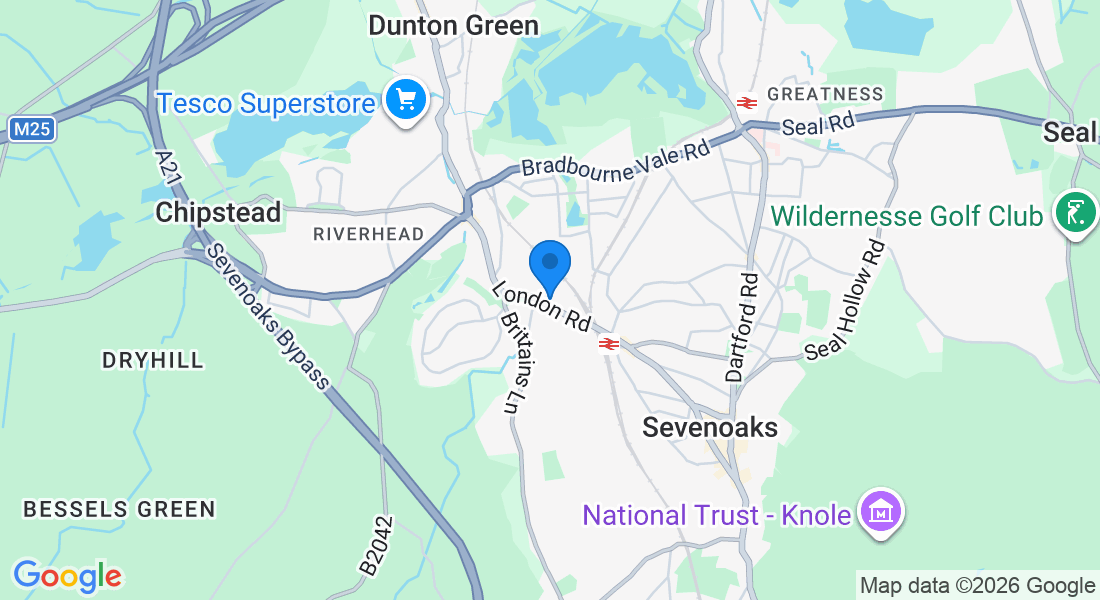
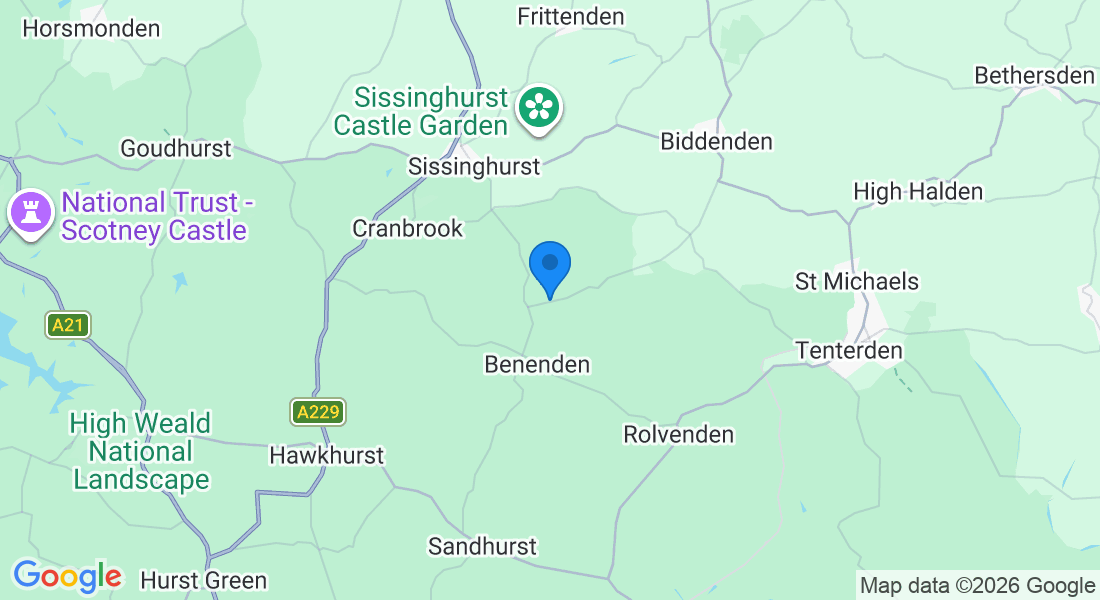
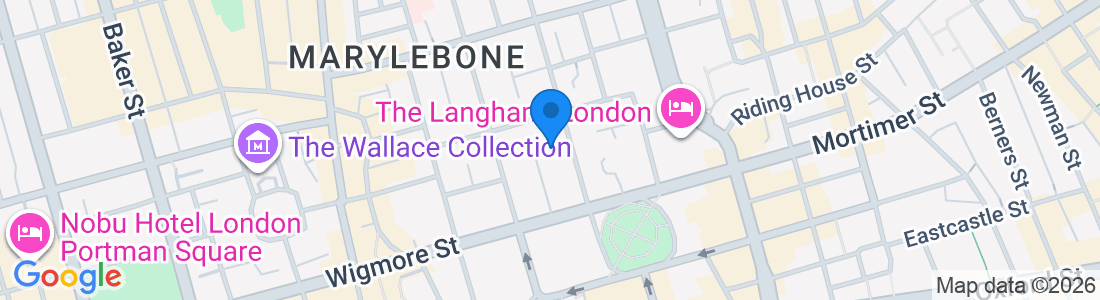
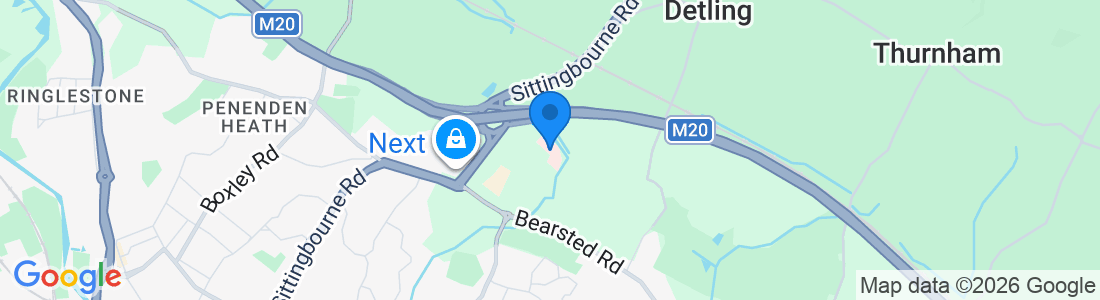
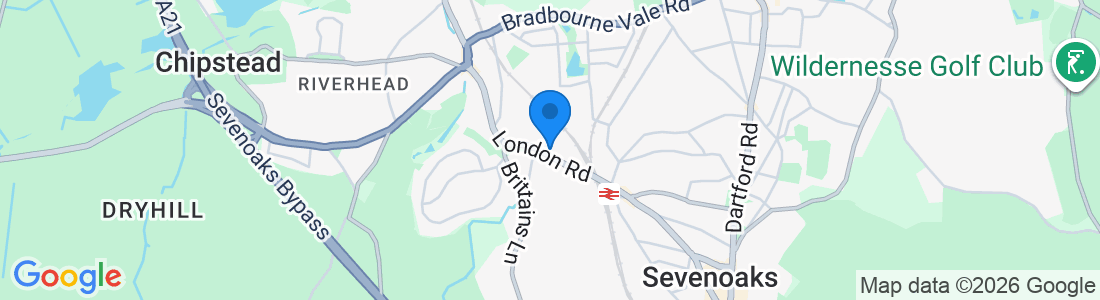
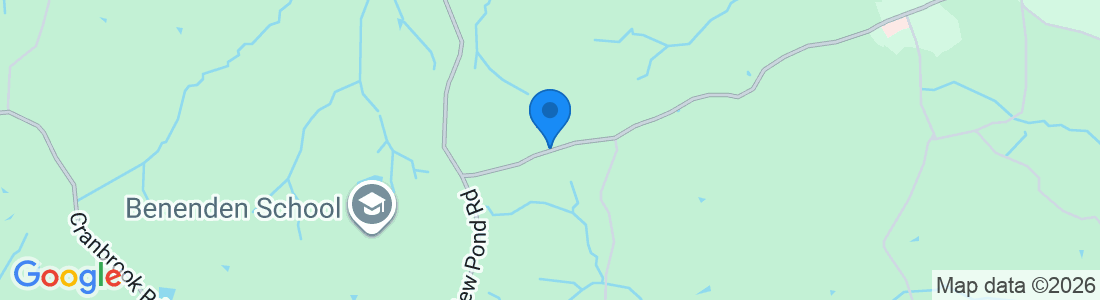
Hospital Locations
Mr Connell consults at multiple locations across Kent and London
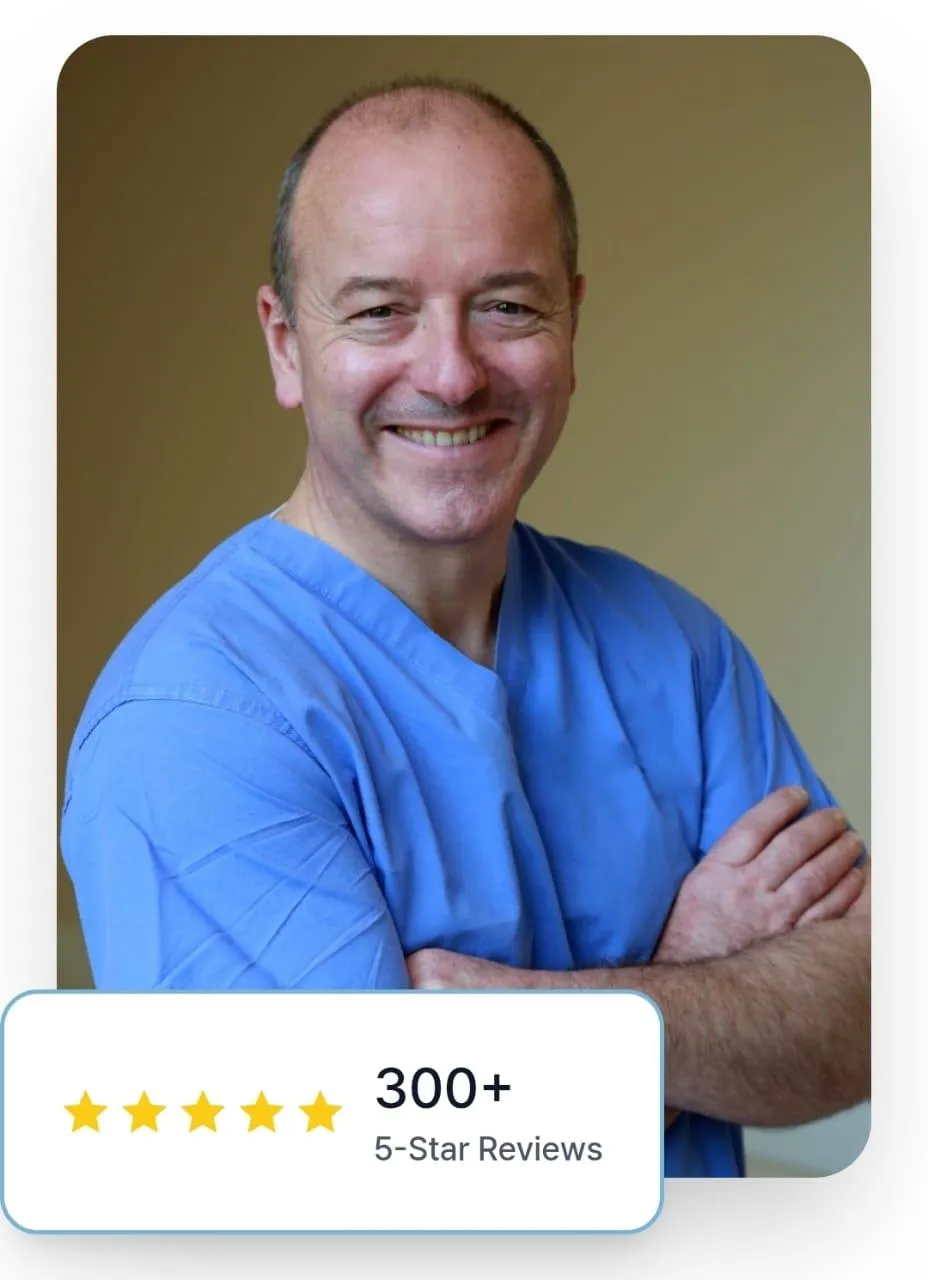
ABOUT
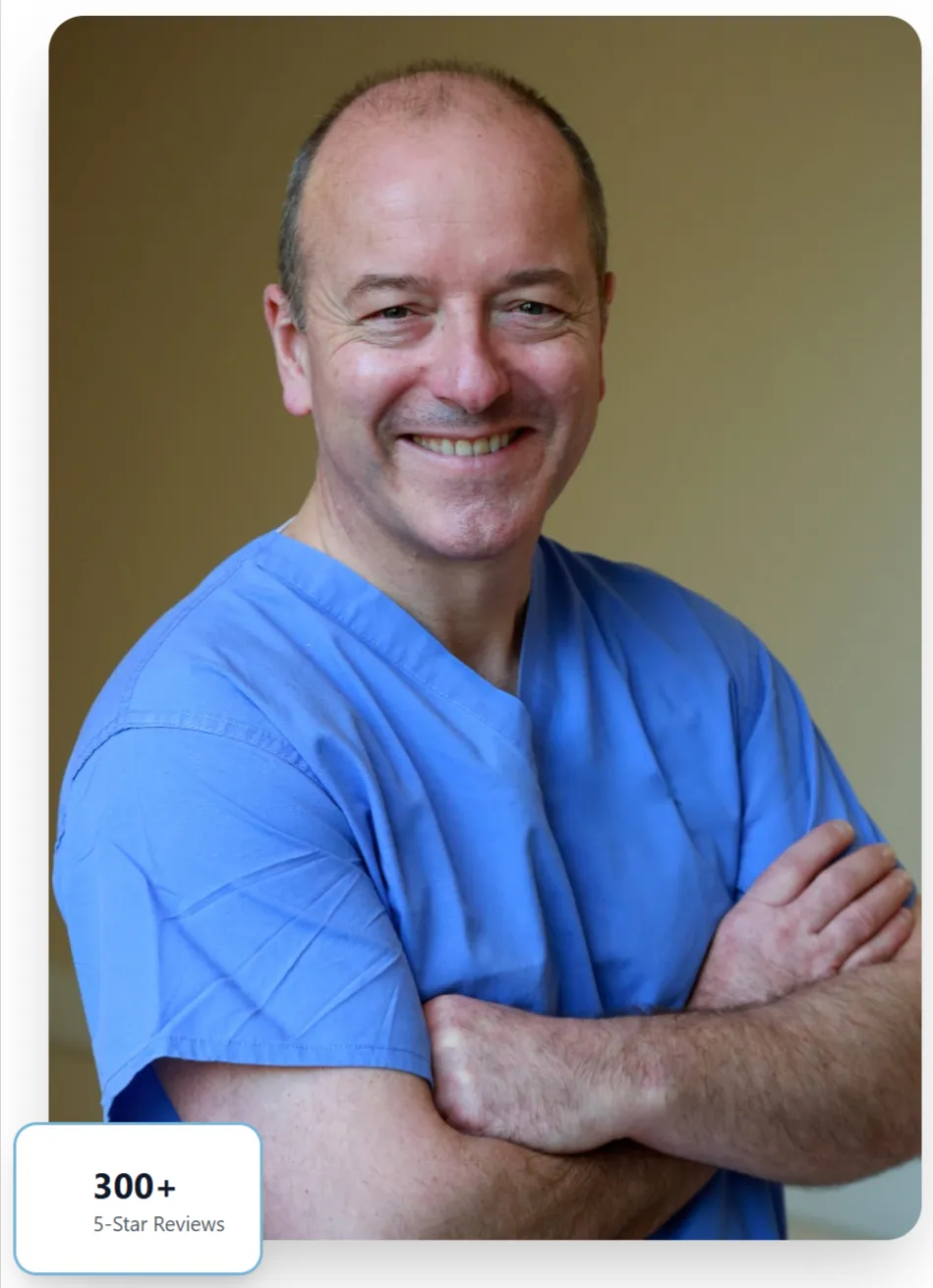
Expert Care You Can Trust
With over 34 years of experience, Mr Rowan Connell is a leading Consultant Gynaecologist based in West Kent, specializing in HRT, urogynaecology, and advanced minimally invasive surgical techniques.
SERVICES
Comprehensive Women's Health
Access detailed information about procedures, recovery guidelines, and what to expect. We provide comprehensive resources to help you make informed decisions about your care.
TESTIMONIALS
What Patients Say
"Mr Connell is approachable, easy to talk to, and a compassionate surgeon. His expertise and care have made a tremendous difference in my life." Read hundreds of 5-star reviews from satisfied patients.
PATIENT INFO
Treatment Information
Access detailed information about procedures, recovery guidelines, and what to expect. We provide comprehensive resources to help you make informed decisions about your care.